Every year, more than 37 million Americans live with diabetes, and nearly 1 in 4 adults don’t even know they have it. For those already diagnosed, managing diabetes at home can feel like a full-time job—balancing medications, meals, activity, and foot care, all while avoiding complications.
But small, consistent habits make a huge difference. When patients and caregivers establish a solid routine for medication management, daily foot checks, and healthy meal planning, diabetes becomes more predictable—and life becomes more manageable.
This article breaks down the daily routines that protect your long-term health, showing how home visits and medication reviews can simplify care, reduce risk, and restore confidence in managing diabetes right where you live.
Building Confidence in Daily Diabetes Care
Managing diabetes at home isn’t just about checking blood sugar—it’s about building a rhythm. Consistency turns tasks into habits, and habits turn into health protection.
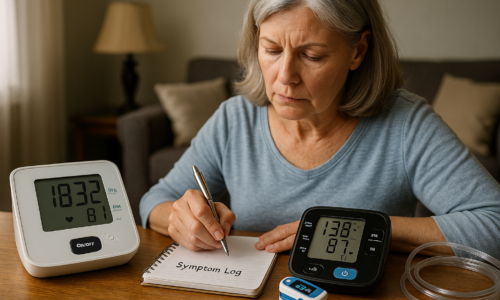
Start by setting specific times for taking medications and checking glucose levels. Keep supplies—test strips, meters, lancets, and insulin—organized and easily accessible. Label your insulin pens or oral medications clearly, and use a weekly pill organizer to stay on track.
A stable routine reduces skipped doses, stabilizes glucose levels, and helps your care team spot trends before they become problems. It’s not about perfection; it’s about consistency.
Medication Management Made Simple
Medication errors are one of the most common reasons for blood sugar spikes and hospital visits among people with diabetes. Understanding what each medication does, when to take it, and how it interacts with meals or other prescriptions is essential.
Always take insulin and oral diabetes medications exactly as prescribed. Timing matters—especially with meals. Missing or doubling a dose can lead to dangerous highs or lows.
Keep a list of every medication you take, including vitamins and over-the-counter drugs. Review it regularly with your healthcare provider to check for potential interactions or dose adjustments. If you notice side effects such as dizziness, swelling, or changes in vision, report them immediately.
At Home Medical Professionals offers medication-review visits, where clinicians review your regimen in person, explain how each medication works, and help simplify complex schedules. These visits often uncover small adjustments that make big improvements in daily control.
Daily Foot Checks: Small Step, Big Protection
Foot health is one of the most overlooked parts of diabetes management, yet poor circulation and nerve damage make feet especially vulnerable. A simple daily foot check can prevent infections, ulcers, and even amputations.
Set aside a few minutes each day to examine your feet under good lighting. Look for redness, blisters, swelling, cuts, or any skin changes. Don’t forget to check between the toes. If mobility is limited, use a mirror or ask a family member or caregiver for help.
Wash your feet daily with warm (not hot) water, dry them gently—especially between the toes—and apply moisturizer to prevent cracking. Always wear shoes and socks that fit well, and never walk barefoot, even indoors.
If you notice any sores, color changes, or numbness, contact your healthcare provider immediately. A quick response can prevent serious complications.
Meal Planning That Works at Home
A balanced meal plan doesn’t mean giving up everything you enjoy—it means learning how to make better choices. The key is consistency: eating at regular times, balancing carbohydrates, and pairing them with lean proteins and healthy fats.
Plan your meals ahead of time to avoid last-minute decisions that lead to poor choices. Use smaller plates to control portions and include a colorful variety of fruits and vegetables. Limit processed foods, sugary drinks, and refined carbs.
For patients managing both diabetes and other conditions like heart disease or kidney issues, a professional dietary consultation can make meal planning much simpler. At Home Medical Professionals can coordinate nutritional guidance as part of your home care plan, ensuring your meals align with your medications and glucose targets.
If you’re using insulin or medications that affect blood sugar, remember that timing matters—try to eat meals consistently and check your glucose before and after to understand how your body responds.
The Role of Home Visits and Care Coordination
Managing diabetes alone can be overwhelming, especially for older adults or caregivers supporting a loved one. Home visits provide personalized support that integrates education, medication review, and symptom monitoring in one setting.
During a home visit, clinicians can check blood glucose logs, inspect feet, review medication techniques (like insulin pen use or glucometer calibration), and identify environmental risks such as poor lighting, clutter, or unsafe storage.
Telehealth follow-ups extend that connection between visits, offering quick check-ins to review blood sugar readings, adjust medications, or reinforce meal and foot care routines. Together, these touchpoints build confidence and help prevent costly complications.
Using Technology to Stay on Track
Smart glucose meters, continuous glucose monitors (CGMs), and mobile health apps make tracking easier than ever. Many devices sync automatically with your smartphone or care team’s portal, giving you instant insight into patterns and helping providers fine-tune treatment remotely.
Set reminders on your phone for medication times, meals, and glucose checks. Some devices even offer trend analysis, predicting potential highs or lows before they happen.
However, technology only helps if it fits your lifestyle. Choose systems you find easy to use and understand. Simplicity leads to consistency, and consistency leads to better control.
Empowering Caregivers and Family Members
For caregivers, managing someone’s diabetes means balancing support with respect for independence. Encourage routine checks and meal planning without taking over completely. Share calendars, set shared reminders, and keep communication open with the healthcare team.
Home care clinicians can also train family members to recognize early signs of hypoglycemia or infection, respond quickly, and document readings accurately. Empowering caregivers strengthens the whole circle of care—and ensures the patient never feels alone in the process.
Creating a Sustainable Home Routine
Successful diabetes management at home depends on structure. Combine daily foot checks, medication timing, meal planning, and glucose monitoring into a single daily routine. Keep tools and supplies organized in a central area, and record results in one place—paper log, app, or digital dashboard.
Small adjustments like preparing weekly meal plans, setting alarms for medication, or laying out foot-care supplies at night reduce friction and increase follow-through. Over time, these habits become second nature, protecting health and improving quality of life.
Managing diabetes at home is about more than blood sugar readings—it’s about living fully, safely, and confidently. With consistent medication management, daily foot checks, and thoughtful meal planning, you take charge of your condition instead of letting it control you.
This week, commit to one step toward better balance: organize your medication schedule, create a foot check reminder, or plan your meals for the next three days. Each small action brings lasting results.
If you’d like extra support, reach out to At Home Medical Professionals and ask about a medication-review visit. Together, we’ll help you simplify your routine, strengthen your confidence, and make your home the best place for better health.