Nearly 40% of adults over age 65 take five or more prescriptions every day, and many add supplements or over-the-counter medicines on top of that. While each medication may have a purpose, the combination can create confusion, side effects, or dangerous interactions. This growing challenge—known as polypharmacy—is one of the leading causes of preventable hospital visits among older adults.
The good news: with regular medication-review visits and open deprescribing conversations, seniors and caregivers can regain control, simplify routines, and stay safer at home. This post explores practical steps to streamline medication lists, avoid common risks, and make every pill truly count.
Understanding Polypharmacy
Polypharmacy simply means taking multiple medications at once, but its impact goes far beyond the numbers. As we age, our metabolism slows, kidneys and liver process drugs differently, and side effects can become more severe. Combining several prescriptions—especially from different specialists—can lead to fatigue, dizziness, confusion, or falls.
Even well-intentioned medication changes can pile up over time. A drug started years ago for one condition may no longer be needed, yet remains on the list. That’s why a clear, updated medication record—and a periodic “clean-up” through a professional review—is essential.
The Brown-Bag Review: A Simple Starting Point
A brown-bag review is exactly what it sounds like: gather all your medications—prescriptions, vitamins, supplements, inhalers, ointments, and over-the-counter pills—place them in a bag, and bring them to your appointment.
During a brown-bag session, a clinician or pharmacist will:
-
Examine every label and dosage for accuracy and duplicates
-
Identify expired, unnecessary, or conflicting drugs
-
Discuss when and how each medication should be taken
-
Check for drug-to-drug or drug-to-food interactions
-
Simplify schedules to reduce confusion and missed doses
This visual, hands-on process often reveals surprises—multiple bottles of the same medication, overlapping pain relievers, or supplements that interfere with prescriptions. A single visit can clarify your entire regimen.
Deprescribing: When Less Is More
Deprescribing doesn’t mean stopping medications recklessly—it means thoughtfully and safely reducing or discontinuing drugs that are no longer beneficial or may cause harm.
Healthcare providers review each medication’s purpose, weighing benefits against side effects and current health goals. Sometimes, a dosage adjustment or substitution is enough; other times, a medication can be phased out altogether.
Deprescribing requires teamwork: patients, caregivers, physicians, and pharmacists working together to balance treatment with quality of life. For many seniors, the result is improved energy, clearer thinking, and fewer falls or ER visits.
Creating and Maintaining a Safe Medication List
An accurate medication list is your foundation for safety. Keep it updated, printed, and easily accessible in case of emergencies or new appointments. It should include:
-
The name, strength, and dosage of each medication
-
When and why it’s taken
-
Who prescribed it
-
Start and stop dates if known
-
Notes about side effects or reactions
Store the list in a visible place—on the refrigerator, near your medication station, or shared electronically with family caregivers. Review it after every hospital stay, medication refill, or doctor visit.
At Home Medical Professionals offers medication-review appointments designed to help seniors create and maintain this list, reconcile differences between provider records, and ensure safe coordination across all specialists.
Common Red Flags to Watch For
If you or a loved one experience any of the following, it may signal medication overload or interactions that need review:
-
Dizziness, lightheadedness, or frequent falls
-
Sudden confusion or memory changes
-
New swelling, fatigue, or gastrointestinal issues
-
Blurred vision or difficulty concentrating
-
Taking the same medication from two prescribers
-
Skipped doses due to complicated schedules
Don’t ignore these signs. Often, they resolve once the medication list is simplified and side effects are properly managed.
Partnering with Home-Based Care for Safer Management
For seniors managing complex regimens, in-home visits provide the safest and most comfortable way to review medications. A visiting clinician can assess medication storage, verify correct usage, and identify potential barriers—like reading small print or opening childproof caps.
Telehealth follow-ups allow continued monitoring and easy communication with pharmacists or physicians. These home-based services reduce errors, prevent hospitalizations, and bring peace of mind to patients and families alike.
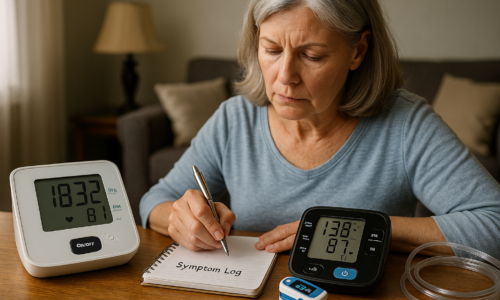
The Caregiver’s Role
Caregivers are the first line of defense against medication errors. Keep a shared log of every dose given, note side effects, and encourage open discussions with healthcare professionals. Bring the brown-bag list to each appointment and advocate for deprescribing conversations when medications seem redundant or burdensome.
Simple tools—like pill organizers, reminder apps, and medication charts—can dramatically reduce stress and confusion. Empowering caregivers strengthens the entire care plan and keeps seniors safer at home.
Conclusion
Polypharmacy doesn’t have to be inevitable. With regular reviews, clear communication, and proactive deprescribing, older adults can reduce medication risks while maintaining comfort and independence.
This week, take one small step: gather all medications in a single place and prepare for your own brown-bag review. It’s one of the simplest ways to uncover hidden risks and ensure every prescription truly supports your health goals.
To learn more or schedule a personalized medication-review appointment, contact At Home Medical Professionals. Together, we’ll help you build a safer, simpler, and more effective medication plan—one that supports longevity, clarity, and confidence.